Antiarrhythmic agent

Antiarrhythmic agents are a group of pharmaceuticals that are used to suppress fast rhythms of the heart (cardiac arrhythmias), such as atrial fibrillation, atrial flutter, ventricular tachycardia, and ventricular fibrillation.
While the use of antiarrhythmic agents to suppress atrial arrhythmias (atrial fibrillation and atrial flutter) is still in practice, it is unclear whether suppression of atrial arrhythmias will prolong life.[1][2]
In the past, it was believed that following myocardial infarction (heart attack), suppression of ventricular arrhythmias would prolong life. However, large clinical trials such as CAST and CAPS found that suppression of these arrhythmias would ironically increase mortality,[3][4] which may happen due to the proarrhythmic effect these drugs may have.[4]
In individuals with atrial fibrillation, antiarrhythmics are still used to suppress arrhythmias. This is often done to relieve the symptoms that may be associated with the loss of the atrial component to ventricular filling (atrial kick) that is due to atrial fibrillation or flutter.
In individuals with ventricular arrhythmias, antiarrhythmic agents are often still in use to suppress arrhythmias. In this case, the patient may have frequent arrhythmic events or be at high risk for ventricular arrhythmias. Antiarrhythmic agents may be considered the first-line therapy in the prevention of sudden death in certain forms of structural heart disease, and failure of these agents to suppress arrhythmias may lead to implantation of an implantable cardioverter-defibrillator (ICD).
Many attempts have been made to classify antiarrhythmic agents. The problem arises from the fact that many of the antiarrhythmic agents have multiple modes of action, making any classification imprecise.
Contents |
Vaughan Williams antiarrhythmic classification
The Vaughan Williams classification, introduced in 1970,[5] is one of the most widely used classification schemes for antiarrhythmic agents. This scheme classifies a drug based on the primary mechanism of its antiarrhythmic effect. However, its dependence on primary mechanism is one of the limitations of the VW classification, since many antiarrhythmic agents have multiple action mechanisms. Amiodarone, for example, has effects consistent with all of the first four classes. Another limitation is the lack of consideration within the VW classification system for the effects of drug metabolites. Procainamide—a class Ia agent whose metabolite N-acetyl procainamide (NAPA) has a class III action—is one such example. A historical limitation was that drugs such as digoxin and adenosine – important antiarrhythmic agents – had no place at all in the VW classification system. This has since been rectified by the inclusion of class V.
There are five main classes in the Vaughan Williams classification of antiarrhythmic agents:
- Class I agents interfere with the sodium (Na+) channel.
- Class II agents are anti-sympathetic nervous system agents. Most agents in this class are beta blockers.
- Class III agents affect potassium (K+) efflux.
- Class IV agents affect calcium channels and the AV node.
- Class V agents work by other or unknown mechanisms.
Overview table
| Class | Known as | Examples | Mechanism | Clinical uses [6] |
|---|---|---|---|---|
| Ia | fast-channel blockers |
|
(Na+) channel block (intermediate association/dissociation) |
|
| Ib |
|
(Na+) channel block (fast association/dissociation) |
|
|
| Ic |
|
(Na+) channel block (slow association/dissociation) |
|
|
| II | Beta-blockers |
|
beta blocking Propranolol also shows some class I action |
|
| III |
|
K+ channel blocker
Sotalol is also a beta blocker[7] |
|
|
| IV | slow-channel blockers |
|
Ca2+ channel blocker |
|
| V | Work by other or unknown mechanisms (Direct nodal inhibition). | Used in supraventricular arrhythmias, especially in Heart Failure with Atrial Fibrillation, contraindicated in ventricular arrhythmias. |
Class I agents
The class I antiarrhythmic agents interfere with the sodium channel. Class I agents are grouped by what effect they have on the Na+ channel, and what effect they have on cardiac action potentials.
Class 1 agents are called Membrane Stabilizing agents. The 'stabilizing' is the word used to describe the decrease of excitogenicity of the plasma membrane which is brought about by these agents. (Also noteworthy is that a few class 2 agents like propranolol also have a membrane stabilizing effect.)
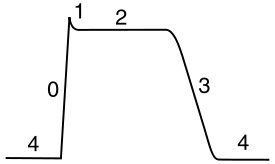
Class I agents are divided into three groups (1a, 1b and 1c) based upon their effect on the length of the action potential.[8][9]
- 1A lengthens the action potential (right shift)
- 1B shortens the action potential (left shift)
- 1C does not significantly affect the action potential (no shift)
 Class Ia agent decreasing Vmax, thereby increasing action potential duration. |
 Class Ib |
 Class Ic |
Class II agents
Class II agents are conventional beta blockers. They act by blocking the effects of catecholamines at the β1-adrenergic receptors, thereby decreasing sympathetic activity on the heart. These agents are particularly useful in the treatment of supraventricular tachycardias. They decrease conduction through the AV node.
Class II agents include atenolol, esmolol, propranolol, and metoprolol.
Class III agents

Class III agents predominantly block the potassium channels, thereby prolonging repolarization.[10] Since these agents do not affect the sodium channel, conduction velocity is not decreased. The prolongation of the action potential duration and refractory period, combined with the maintenance of normal conduction velocity, prevent re-entrant arrhythmias. (The re-entrant rhythm is less likely to interact with tissue that has become refractory). Drugs include: amiodarone, ibutilide, sotalol, dofetilide, and dronedarone.
Class IV agents
Class IV agents are slow calcium channel blockers. They decrease conduction through the AV node, and shorten phase two (the plateau) of the cardiac action potential. They thus reduce the contractility of the heart, so may be inappropriate in heart failure. However, in contrast to beta blockers, they allow the body to retain adrenergic control of heart rate and contractility.
Class IV agents include verapamil and diltiazem.
Other agents ("Class V")
Since the development of the original Vaughan-Williams classification system, additional agents have been used that don't fit cleanly into categories I through IV.
Some sources use the term "Class V".[11] However, they are more frequently identified by their precise mechanism.
Agents include:
- Digoxin, which decreases conduction of electrical impulses through the AV node and increases vagal activity via its central action on the central nervous system.
- Adenosine[12]
- Magnesium sulfate,[13] which has been used for torsades de pointes.[14][15]
Sicilian Gambit classification
Another approach, known as the "Sicilian Gambit", placed a greater approach on the underlying mechanism.[16][17][18]
It presents the drugs on two axes, instead of one, and is presented in tabular form. On the Y axis, each drug is listed, in approximately the Vaughan Williams order. On the X axis, the channels, receptors, pumps, and clinical effects are listed for each drug, with the results listed in a grid. It is therefore not a true classification in that it does not aggregate drugs into categories.[19]
Trials
The Cardiac Arrhythmia Suppression Trial (CAST trial) [20] (published in 1989) was a medical study that demonstrated that some class 1 anti-arrhythmic drugs were not helpful to people suffering from ventricular premature depolarization. Specifically, for populations of recent heart attack survivors, the study observed lower mortality in a control population than in populations treated with encainide, flecainide or moricizine (all class 1c drugs). The Cardiac Arrhythmia Pilot Study (CAPS, published in 1986) was another study to investigate arrhythmias.
Other major trials examining antiarrhythmic drugs include Antiarrhythmics Versus Implantable Defibrillators (AVID), and the Atrial Fibrillation Follow-Up Investigation of Rhythm Management (AFFIRM), which compared antiarrhythmic drugs with drugs which controlled inappropriately rapid and irregular heart rate. In both trials, the arrhythmic drugs were less effective than the alternative.[21]
Mnemonics
Mnemonic for Class I-IV agents: SoBe PoCa (SOBE as in South Beach or the drink, POCA as in Polka)
Also - remembering that of all anti-arrhythmics "some block potassium channels" can help you:
- Class I "Some" = S = Sodium
- Class II "Block" = B =Beta blockers
- Class III "Potassium" = Potassium channel blockers
- Class IV "Channels" = C =Calcium channel blockers
Specific drugs:
- Class I agents:
- Class IA “Double Quarter Pounder” (Disopyramide, Quinidine, Procainamide)
- Class IB “Lettuce, Tomato, Mayo, Pickles” (Lidocaine, Tocainide, Mexilitine, Phenytoin)
- Class IC “More Fries Please” (Moricizine, Flecainide, Propafenone).
- Class III agents: "A Big Dog Is Scary" (Amiodarone, Bretylium, Dofetilide, Ibutilide, Sotalol).
- Class IV: Calcium channel blockers are verapamil and diltiazem. NB: Nifedipine is not cardioselective and is therefore not a class IV anti-arrhythmic even though dihydropyridines are considered Ca2+ channel blockers].
See also
- Action potential
- Cardiac action potential
- Electrocardiogram
- Proarrhythmic agent
References
- ↑ Wyse D, Waldo A, DiMarco J, Domanski M, Rosenberg Y, Schron E, Kellen J, Greene H, Mickel M, Dalquist J, Corley S (2002). "A comparison of rate control and rhythm control in patients with atrial fibrillation". N Engl J Med 347 (23): 1825–33. doi:10.1056/NEJMoa021328. PMID 12466506.
- ↑ Nichol G, McAlister F, Pham B, Laupacis A, Shea B, Green M, Tang A, Wells G (2002). "Meta-analysis of randomised controlled trials of the effectiveness of antiarrhythmic agents at promoting sinus rhythm in patients with atrial fibrillation". Heart 87 (6): 535–43. doi:10.1136/heart.87.6.535. PMID 12010934.
- ↑ Wyse DG, Morganroth J, Ledingham R, Denes P, Hallstrom A, Mitchell LB, Epstein AE, Woosley RL, Capone R (1994). "New insights into the definition and meaning of proarrhythmia during initiation of antiarrhythmic drug therapy from the Cardiac Arrhythmia Suppression Trial and its pilot study. The CAST and CAPS Investigators". J Am Coll Cardiol. 23 (5): 1130–40. doi:10.1016/0735-1097(94)90601-7. PMID 8144779.
- ↑ 4.0 4.1 "Effect of the antiarrhythmic agent moricizine on survival after myocardial infarction. The Cardiac Arrhythmia Suppression Trial II Investigators". N Engl J Med 327 (4): 227–33. 1992. doi:10.1056/NEJM199207233270403. PMID 1377359.
- ↑ Vaughan Williams EM. "Classification of anti-arrhythmic drugs." In: Symposium on Cardiac Arrhythmias, Sandfte E, Flensted-Jensen E, Olesen KH eds. Sweden, AB ASTRA, Södertälje, 1970;449-472.
- ↑ Unless else specified in boxes, then ref is: Rang, H. P. (2003). Pharmacology. Edinburgh: Churchill Livingstone. ISBN 0-443-07145-4.
- ↑ Kulmatycki KM, Abouchehade K, Sattari S, Jamali F (May 2001). "Drug-disease interactions: reduced beta-adrenergic and potassium channel antagonist activities of sotalol in the presence of acute and chronic inflammatory conditions in the rat". Br. J. Pharmacol. 133 (2): 286–94. doi:10.1038/sj.bjp.0704067. PMID 11350865.
- ↑ Milne JR, Hellestrand KJ, Bexton RS, Burnett PJ, Debbas NM, Camm AJ (February 1984). "Class 1 antiarrhythmic drugs--characteristic electrocardiographic differences when assessed by atrial and ventricular pacing". Eur. Heart J. 5 (2): 99–107. PMID 6723689. http://eurheartj.oxfordjournals.org/cgi/pmidlookup?view=long&pmid=6723689.
- ↑ Trevor, Anthony J.; Katzung, Bertram G. (2003). Pharmacology. New York: Lange Medical Books/McGraw-Hill, Medical Publishing Division. pp. 43. ISBN 0-07-139930-5.
- ↑ Lenz TL, Hilleman DE, Department of Cardiology, Creighton University, Omaha, Nebraska. Dofetilide, a New Class III Antiarrhythmic Agent. Pharmacotherapy 20(7):776-786, 2000. (Medline abstract)
- ↑ Fogoros, Richard N. (1999). Electrophysiologic testing. Oxford: Blackwell Science. pp. 27. ISBN 0-632-04325-3.
- ↑ Conti JB, Belardinelli L, Utterback DB, Curtis AB (March 1995). "Endogenous adenosine is an antiarrhythmic agent". Circulation 91 (6): 1761–7. PMID 7882485. http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=7882485.
- ↑ Brugada P (July 2000). "Magnesium: an antiarrhythmic drug, but only against very specific arrhythmias". Eur. Heart J. 21 (14): 1116. doi:10.1053/euhj.2000.2142. PMID 10924290. http://eurheartj.oxfordjournals.org/cgi/pmidlookup?view=long&pmid=10924290.
- ↑ Hoshino K, Ogawa K, Hishitani T, Isobe T, Eto Y (October 2004). "Optimal administration dosage of magnesium sulfate for torsades de pointes in children with long QT syndrome". J Am Coll Nutr 23 (5): 497S–500S. PMID 15466950. http://www.jacn.org/cgi/pmidlookup?view=long&pmid=15466950.
- ↑ Hoshino K, Ogawa K, Hishitani T, Isobe T, Etoh Y (April 2006). "Successful uses of magnesium sulfate for torsades de pointes in children with long QT syndrome". Pediatr Int 48 (2): 112–7. doi:10.1111/j.1442-200X.2006.02177.x. PMID 16635167. http://www3.interscience.wiley.com/resolve/openurl?genre=article&sid=nlm:pubmed&issn=1328-8067&date=2006&volume=48&issue=2&spage=112.
- ↑ "The 'Sicilian Gambit'. A new approach to the classification of antiarrhythmic drugs based on their actions on arrhythmogenic mechanisms. The Task Force of the Working Group on Arrhythmias of the European Society of Cardiology". Eur. Heart J. 12 (10): 1112–31. October 1991. PMID 1723682. http://eurheartj.oxfordjournals.org/cgi/pmidlookup?view=long&pmid=1723682.
- ↑ Vaughan Williams EM (November 1992). "Classifying antiarrhythmic actions: by facts or speculation". J Clin Pharmacol 32 (11): 964–77. PMID 1474169. http://jcp.sagepub.com/cgi/pmidlookup?view=long&pmid=1474169.
- ↑ "Milestones in the Evolution of the Study of Arrhythmias". http://www.medscape.com/viewarticle/412798_3. Retrieved 2008-07-31.
- ↑ Fogoros, Richard N. (1997). Antiarrhythmic drugs: a practical guide. Oxford: Blackwell Science. pp. 49. ISBN 0-86542-532-9.
- ↑ Entry on Clinical Trials.gov
- ↑ "Dr. D. George Wyse - antiarrhythmic drugs". http://www.calgaryhealthregion.ca/newslink/region_news/2007/2007-08-17_george_wyse.html. Retrieved 2008-08-27.
|
||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||||||||||